|
MimiVax, Inc. is developing immunotherapeutic vaccines and targeted therapies for treating cancers and preventing recurrence. The company’s lead agent, SurVaxM, targets survivin, a cell-survival protein expressed in cancer cells.
Read more in Nature BioPharma Dealmakers
0 Comments
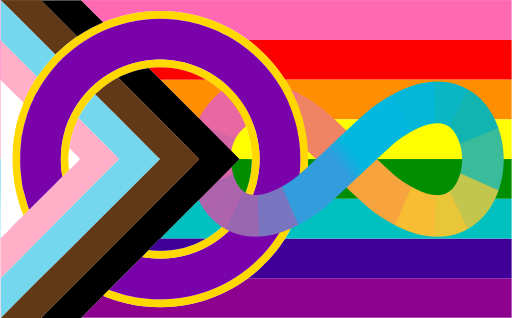
In 2021/2022, 3.3% of the UK population identified as lesbian, gay or bisexual, 0.5% identified as transgender and 0.06% identified as non-binary. Globally, up to 1.7% of the population is intersex. Despite these numbers, there is a lack of research into how treatments affect people across the spectrum of sexuality and gender, and this has potential to put people from these communities at risk. Diversity in clinical research is vital in order to ensure that the study results are relevant to as broad a population as possible, and this includes involving people from LGBTQIA+ communities. Accessing the widest possible population will also allow companies to recruit enough people for studies, and therefore move drugs through the development process more quickly, speeding up the time it takes to get to market and into the hands of patients. Improving the inclusivity of clinical research will help everyone to gain equitable access to the most effective and safest forms of treatment. Barriers to taking part in clinical trials For LGBTQIA+ people, a range of barriers can contribute to making clinical research a less viable option for them. Loss of trust Many people from the LGBTQIA+ community have had poor experience(s) when accessing and experiencing healthcare. Negative experiences can fuel mis- and dis-trust of healthcare both as a system and the healthcare professionals that work within it. These experiences are highly likely to likely to impact willingness to take part in clinical trials. From a Stonewall survey:
Other issues include:
The impact of gender and sexuality The barriers already discussed show why LGBTQIA+ people overall may be less likely to accept or interact with medical interventions. It goes further, though – the impact of gender and sexuality on healthcare is complex, and it crosses biology, neurodiversity, culture, sociology and current and past medical interactions. These are a few examples:
Access to clinical trials People in the LGBTQIA+ community are more likely to be unemployed, work part-time, or have a lower-paid job. This has an impact on whether they can afford to travel to clinical trial sites or take time off for clinic visits. Neurodiversity comes with issues of sensory overload and difficulties in processing or remembering information, all of which make the unfamiliarity of a clinical trial site harder to navigate. Binary inclusion/exclusion criteria can also reduce the ability of trans and non-binary people to take part in clinical trials. Some clinical trials also actively exclude gay men and lesbians. Building better clinical trials Making changes improve access for LGBTQIA+ people to clinical trials. One key change is queering the language. Talking about studies using the binary terms men and women can exclude trans, non-binary and intersex people. Changing the wording, for example from men to people with a prostate or from women to people with ovaries, isn’t about erasing men and women and the language associated with them, it’s about being specific and accurate with the language that we use. This will broaden the population of people who see that they are able to participate, and make the results more applicable to the general population. As an example, contraception wording in informed consent forms is often tailored towards heterosexual cisgender couples:
Some studies do need exclusion criteria, for example if hormone treatments cause drug-drug interactions with the study drug. In this case, the protocol should be worded to exclude the treatments and not the groups of people.
Other changes, some of which are simple and low or no cost, could make major differences to the inclusivity of a study:
By involving more LGBTQIA+ people in studies and making them welcome, companies developing new drugs can improve the diversity of their clinical trials and improve access to drugs for all. To learn more about why diversity in clinical research is so important, read my piece on Pharma Sources. With thanks to Heidi Green, Director of Health Research Equity, Chloe Stephenson, Research and Insights Manager, and all of the rest of the COUCH Health team Randomised controlled trials (RCTs), where study participants are randomly allocated to an experimental group or a control group, became the 'gold standard' of clinical research in the mid-20th century. [1] RCTs have historically enrolled proportionally more white men than people from other groups, with the thinking, at least in part, being that the results could be extrapolated to all populations. Subsequent research, however, has shown that this is not the case, as underrepresented groups may have different responses to the disease or drug, based on social, cultural and other contexts. [2] Diversity in clinical trials, which is about so much more than differences in biology, is therefore an essential part of ensuring that everyone has equitable access to the most effective and safest approaches to treatment.
Read more at Pharma Sources. Read the article here.
Read the article here.
In 2015, at the United Nations Climate Change Conference (COP21), 196 countries adopted the Paris Agreement to limit global warming to no more than 1.5 °C. This requires countries to cut emissions by at least 45% compared with 2010 levels, and reach net zero by 2050. However, the current commitments from this coalition of countries fall far short; based on current plans, rather than falling, emissions will increase by almost 30% by 2030. It's vital that companies, as well as governments, get behind the goal of net zero as soon as possible.
Read more at Pharma Sources. |
Archives
July 2024
Categories |
 RSS Feed
RSS Feed
